
Understanding Certificate of Need (CON) in Healthcare
From the CHAP Boardroom
Written by Michael Rovinsky | CHAP BoD & VP of Strategic Planning, Array Advisors
Navigating regulatory frameworks is crucial for community-based healthcare organizations looking to initiate or expand their services. The Certificate of Need (CON) stands as a pivotal regulatory tool in this endeavor, playing a significant role in the planning and delivery of healthcare services. In today’s discussion from the CHAP Boardroom, we delve into the Certificate of Need, exploring its implications and its influence on the landscape of community-based care.
What is a Certificate of Need?
Certificate of Need (CON) is a regulatory mechanism employed by numerous states within the United States to oversee the establishment and expansion of healthcare facilities and services. Originally designed to prevent the overbuilding of hospitals and medical facilities, the scope of CON has broadened to include community-based care, such as home health and home care agencies.
The CON process mandates that healthcare providers secure approval from a state health planning agency before constructing new facilities, introducing new or expanding services, or purchasing major medical equipment. The approval hinges on demonstrating a quantifiable, tangible “need” for the proposed services within the community and that the development or expansion of the services will not have a material adverse impact on existing providers.
The Rationale Behind CON Laws
Support for CON Laws:
- Ensuring Adequate Healthcare Services: CON regulations help maintain an optimal balance of healthcare services, preventing excess capacity while enhancing access to necessary services in underserved areas.
- Controlling Cost: By curbing the expansion of facilities and new services, CON laws aim to avert unnecessary capital expenditures that could escalate healthcare costs.
- Promoting Quality Care: These laws support a regulated expansion process, encouraging facilities to focus on quality improvements and adhere to rigorous patient care standards.
- Medicaid Spending and Equitable Care: Several states leverage CON laws to manage Medicaid spending and ensure that healthcare systems provide their fair share of care to indigent and underserved populations.
Criticism of CON Laws:
- Limiting Competition: CON laws may prevent new entrants from competing with established providers, potentially hindering innovation and efficiency in the provision of healthcare services.
- Questioning Cost Impact: With many healthcare payments now fixed through insurance plans or bundled services, any increase in charges implemented by providers to offset declines in utilization caused by the unnecessary duplication of services is unlikely to lead to higher costs for consumers.
- Empirical Challenges: Research indicates that states without CON laws, like Texas, do not necessarily experience higher overall healthcare costs, which calls into question the need for these regulations.
CON Laws by State
CON laws varies significantly by state. As of 2022:
- 12 states did not have CON laws.
- 3 states maintained an approval process akin to CON.
- 35 states and Washington D.C. enforced some form of CON program.
- Several states that are reported to still have CON laws, such as Florida and South Carolina, have significantly scaled them back to only apply to select services, such as long-term care and/or home health services.
For more detailed information on the status of CON laws by state, visit National Conference of State Legislatures.
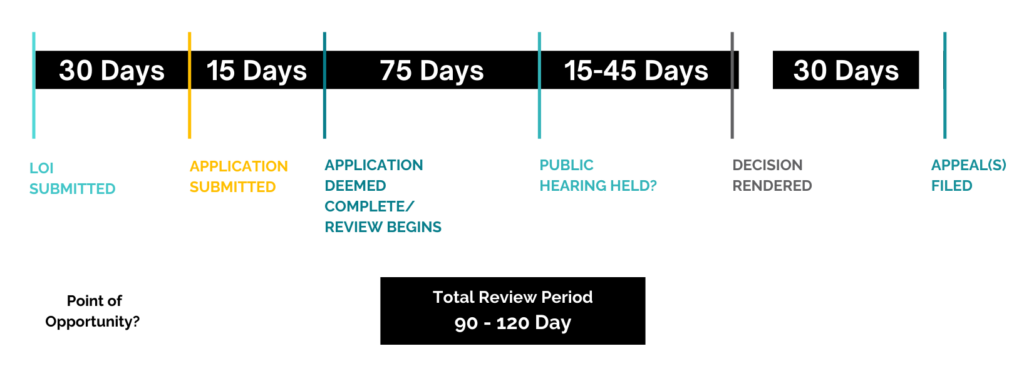
Typical CON Submission and Review Process
Review Criteria Needed for a CON Application
CON applications are usually reviewed under a set of standard review criteria. Typical review criteria may include, but not be limited to:
- Need: Demonstrating an unmet community need for the proposed service.
- Accessibility: Improving access to care by overcoming geographic, financial, cultural, and racial barriers.
- Quality of Care: Adhering to high standards, including staff qualifications and quality improvement measures.
- Continuity of Care: Ensuring coordinated care across various settings.
- Acceptability: Gaining community support and ensuring the project aligns with the target population’s needs.
- Financial Feasibility: Demonstrating the project’s economic sustainability and assessing its financial impact.
Applicants must document the consistency of the proposed project with these criteria in order to be approved.
In many states, there are proscribed methodologies for determining need and/or the state may calculate and specifically define the need for services. For instance, in one state, the Planning Agency undergoes a detailed analysis to determine the unmet patient need for home health services and, based on that calculation, publishes a report indicating the number of new home health agencies that are needed and can be approved in each county in the state. It is then up to applicants to demonstrate how they plan to meet that need and, assuming more than one application is submitted (a competitive review), based on the other review criteria, why it is the best applicant to be permitted (approved) to do so.
Therein lies the rub, as it becomes an exercise in creative writing, analysis, and documentation to justify the need for the new or expanded service, and some providers and their consultants are better at playing the game (manipulating the data) than others.

Meet the Author
Michael Rovinsky is a healthcare strategist, advisor, and business development executive with more than 37 years of experience providing strategic counsel to senior leadership of healthcare provider organizations. His areas of specialization include strategic, business, and regulatory planning; ambulatory medical facility planning and development; hospital/physician alignment; and partnership development. Of particular relevance here, over the course of his career, Michael has prepared more than 75 CON applications and/or provided expert witness testimony in related regulatory proceedings in 12 states and the District of Columbia.
Michael currently serves as Vice President of Strategic Planning for Array Advisors, the advisory arm of Array Architects, an exclusive healthcare architectural firm. In this role, he leads Array’s strategic analytics team in conducting market assessments and developing volume projections to support master facility plans, as well as completing other strategy, CON, and related projects for clients. Michael also serves as President of Integrity Consulting Group, a healthcare consulting firm he initially founded in 1998. Current work includes developing strategic plans for individual system hospitals and facilitating progress and plan updates of a comprehensive strategic plan he helped develop for a $2 billion multi-hospital regional health system. Previously, Michael served as Associate Principal, Senior Healthcare Market Strategist for Perkins&Will; Director, Southeast Region, for Veralon Partners; Executive Director, Strategic Planning for Kaiser Permanente Health Plan of the Mid-Atlantic States; and as Interim Vice President of Planning for Sacred Heart Health System in Pensacola, FL.
Michael earned a BA in Biology and Psychology from the University of Pennsylvania in 1981 and an MBA in Health Care Management from The Wharton School in 1986. He currently serves on the Boards of the Community Health Accreditation Partner (CHAP), the Wharton Health Care Management Alumni Association, and the Southeast Society for Healthcare Strategy and Market Development.