
The Growing Demand for Age-Friendly Care in the United States
The 4Ms of Age-Friendly Care are Like Making a Cake
By Dr. Khai Nguyen, CHAP National Medical Director
“So, what’s the big deal?” asked a medical student rotating with me in my geriatrics clinic one recent afternoon. I had just completed what I felt was one of my more eloquent didactic lessons on the 4Ms Framework for Age-Friendly Care: What Matters, Mentation, Medications, and Mobility. But the medical student pointed out that they already understood these concepts of “asking patients about their goals of care”, “reviewing their medications”, “checking for cognitive and mental health issues”, and “checking for falls”. Again, remarked “so I don’t get it—why is this 4Ms any different than what I am already doing?”
Appreciating this stimulating discussion, a light bulb went off for me, but since it was nearing lunchtime, this light bulb was one that involved food. I proceeded to ask, “Do you bake much?”
“Yes—I enjoy making desserts,” said the medical student.
“You must enjoy a good tasting cake?” I said.
“Yes, I make a really good chocolate cake!” exclaimed the medical student.
Inquisitively I said, “Let’s think about this like baking a cake. The use of the 4Ms together, every patient, every time, by every provider is the innovation. If I were to ask you to eat these ingredients of flour, chocolate, eggs, and sugar separately, would it taste good or would it be a cake?”
“No, you would need to mix it and bake it together,” retorted the medical student.
“Aha! Just like the ingredients of a cake, we all need to practice the 4Ms of Age-Friendly care together, mixed and bake it into our care—that is when we employ the innovation of these evidence-based practices into our patient visits that make it truly age-friendly care,” I emphatically replied.
When addressing patient needs, we need to remember it’s the combination all the ingredients to form the multilayered innovation which is age-friendly care.
The Problem Facing an Aging Population
For the first time in human history, there are now more people living over the age of 64, then under the age of 5. Major contributors to this are advancements in medical technologies, public health efforts and elevated standards of living and hygiene.
Despite all these advancements, the medical system in the United States remains overwhelmed, understaffed, and outdated (in mindset and healthcare) when trying to handle such a massive influx in the needs of older adult populations. With around 7,000 Geriatricians in the United States, the American Geriatrics Society predicts we will need to nearly double this amount by 2030 – just 8 years away – to meet the growing demand.
Furthermore, according to the World Health Organization, ageism is the most widely acceptable prejudice in the world. It is often not taken as seriously as other forms of discrimination. It can affect older adults’ mental health, lead to social isolation, financial insecurity, decreased quality of life and, for our focus, prejudice in healthcare.
Studies have shown, when Dr’s are given identical case studies, with the same symptoms and same likelihood of recovery, they are far less likely to recommend treatments for older patients than their younger counterparts. We can, should, and will, do better by integrating the evidence-based 4Ms of Age-Friendly Care—this is our opportunity.
How Age Friendly Health Systems Provides a Solution
There has never been a more critical need for Age-Friendly Care in all human history. Research shows that providing older populations with specific, age-friendly care has long reaching benefits including reducing the number of emergency department visits, hospitalizations and readmissions, a reduction in medication-related problems, increased mobility, and early detection of memory issues and depression.
Age-Friendly Care strives to follow an essential set of evidence-based practices that cause no harm and align with what matters most to the older adult and their family and caregivers.
Age-Friendly Health Systems is an initiative of the John A. Hartford Foundation (JAHF) and the Institute for Healthcare Improvement in partnership with the American Hospital Association and Catholic Health Association of the United States. Their initial goal was to spread the 4Ms Framework to 20% of US hospitals by 2020. This initiative exceeded that goal with over 2,800 recognized Age-Friendly Health System participants.
Our health care system needs to work at taking a fresh approach that respects older peoples’ autonomy and decisions to live a happy and fulfilled life according to their own terms.
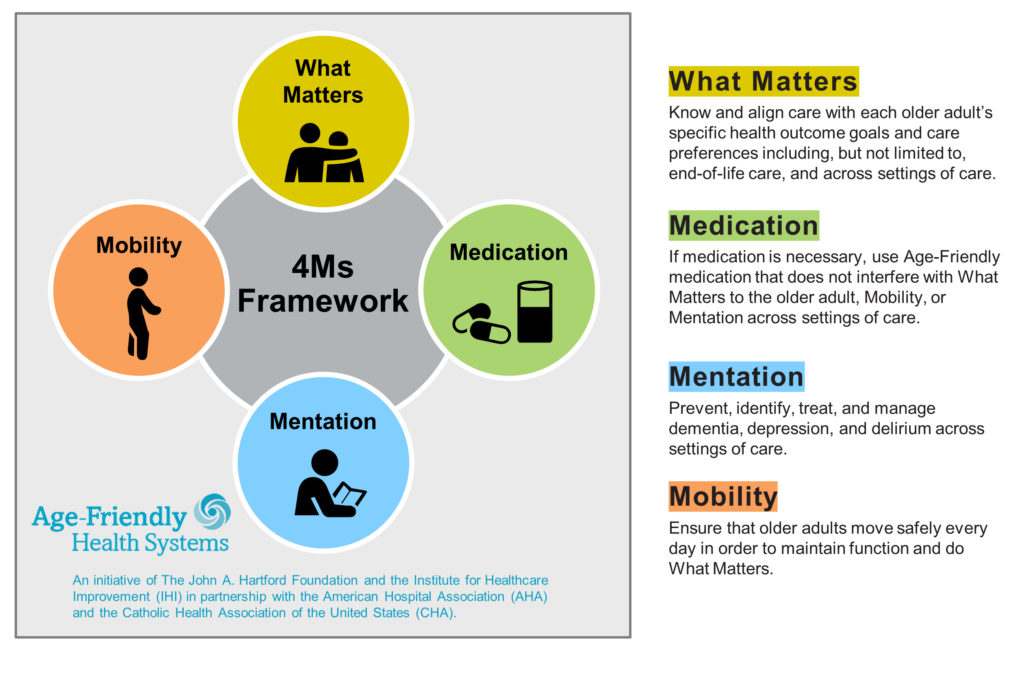
The guiding principles to providing Age-Friendly Care is structured around the 4Ms Framework:
- What Matters to older people with respect to their goals and preferences when getting treatment, end-of-life care and across settings of care.
- Medications that should be avoided or even scaled back as necessary
- An emphasis on Mentation to prevent, identify, treat, and manage dementia, depression, and delirium
- Mobility to ensure older adults can maintain safe mobility, function, and independence
It’s all about mixing all these essential ingredients together that creates something beautiful and when the patient thrives. The synergy of these principles ensures the person is treated as a whole; like treating the patient with the disease, rather than solely treating the disease. More importantly, it is also about respecting what the patient wants.
The general population along with caregivers can view the 4Ms Framework as a guide to be better equipped to assist the growing aging population.
Never has there been a more critical need for education and training on the importance of providing Age-Friendly Care and the 4Ms. Healthcare providers, aging populations, caregivers, and their family members should all be included in what this means.
How CHAP is Supporting Age-Friendly Health Systems in the Home
The United Nations has coined 2021-2030 as the decade of healthy aging. We are at a critical juncture in history where globally governments, society, international agencies, professionals, academia, the media and private sector need to come together to improve the lives of older people.
CHAP has received a grant from the JAHF to develop a certification program that helps bring Age-Friendly Care and the 4Ms Framework to the community and home healthcare setting. This certification would allow for home healthcare agencies with such an Age-Friendly Care certification to manage care for individuals leaving a hospital or health system that is already recognized as an Age-Friendly Health System. Agencies can extend their care to provide for these individuals in their home which allows for more freedom and autonomy for the individual.
What You Can Do to Support an Age-Friendly Movement
To adequately provide for the large demand in Age-Friendly Care, we need to work at educating aging populations and their families on their rights and freedoms of care along with training and certifying health care providers and caregivers on the 4Ms Framework.
Remember, it’s not about all the ingredients in isolation but rather combining them together to make something better for all.