Emergency Preparedness – Hurricanes and Beyond
Emergency Weather Preparedness – Include Hurricanes and Beyond
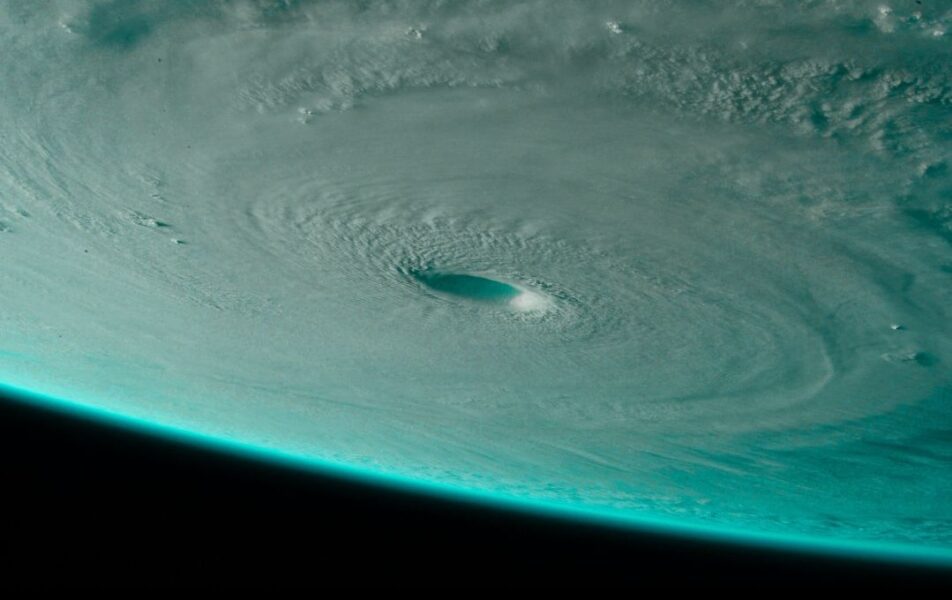
Here we are again at the start of hurricane season which runs from June 1 to November 30. The National Oceanic and Atmospheric Administration (NOAA) is forecasting a more active than average Atlantic storm activity with a 6-in-10 chance of an above-average hurricane season. They also predict an above-normal hurricane season in the Eastern Pacific for 2025, with a 60% chance of an above-normal season. This means that west and east coast healthcare providers could be implementing their emergency preparedness plan sometime between summer and fall related to storm activity.
Outside of the hurricane season, there are plenty of other natural and manmade disasters that could require providers to fully or partially implement their emergency preparedness plan. Current literature states climate change increases the frequency and severity of extreme weather events, making emergency preparedness crucial. Climate change also exacerbates healthcare emergencies which can disrupt healthcare operations, threaten infrastructure, and lead to health risks. So, the question is, “Is your emergency plan up to date and the best it can be?” While the Centers for Medicare and Medicaid Services (CMS) emergency preparedness regulations require providers to minimally review and update their emergency plan every two years, an annual review and update may be in order depending on hazard risk assessment outcomes and actual emergency response from the same or previous year. Given today’s natural and manmade risks, providers cannot afford to operate with an out-of-date emergency plan.
Include The Changing National Landscape
We are five years since the start of the COVID-19 pandemic. In the post-COVID world, the healthcare continuum is still struggling with staffing, reimbursement issues, overstretched systems, and resource shortfalls; all of which are further exacerbated during a disaster or emergency. Additionally, the White House’s transformation of the federal government has reduced programs. The White House has implemented staffing reductions at the Federal Emergency Management Agency (FEMA) and other federal agencies involved in disaster response, shifting more responsibilities to the States and local authorities. This shift in federal policy is intended to empower the States to manage disaster response on their own with only limited federal government reimbursement or support.
Given this current landscape, it is more important than ever for providers to develop and nurture productive relationships with their State or area (county/Parish) Emergency Management Agencies and local Public Health Departments. They need to know who you are as a healthcare provider, your patient’s needs, and how you can assist in a disaster if needed. Your relationship with the state agency also educates them about home-based care patients’ needs during normal operations and during a disaster and recovery. Successful relationships with local, county/Parish, and State agencies are hallmarked by the following attributes:
- Public Health and emergency management agencies/authorities know who you are
- They are aware of both your capabilities/resources and your risks and potential needs
- They know the key information in your emergency response plans that may intersect with their operations.
- You need to know how to contact them for support or information, usually in their emergency operation center.
This relationship may also offer an opportunity to learn about and participate in disaster exercises which is a mode for providers to test their emergency plan.
CMS 1135 Waivers
When the President declares a disaster or emergency under the Stafford Act or National Emergencies Act and the HHS Secretary declares a public health emergency under Section 319 of the Public Health Service Act, the Department of Health and Human Services (HHS) Secretary may, under section 319 of the Public Health Service Act, declare that a Public Health Emergency (PHE) exists in the affected state. Once a PHE is declared, section 1135 of the Social Security Act authorizes the Secretary, among other things, to temporarily modify or waive certain Medicare, Medicaid, Children’s Health Insurance Program (CHIP), and Health Insurance Portability and Accountability Act (HIPAA) requirements that we find are necessary.
CMS can issue blanket waivers when there is a disaster or emergency to prevent access to care gaps for beneficiaries affected by the emergency. If there is no blanket waiver, providers can ask CMS for an individual Section 1135 waiver. This waiver, under section 1135 of the Social Security Act, may temporarily waive or modify certain Medicare, Medicaid, and Children’s Health Insurance Program (CHIP) requirements. Examples of waived items can include:
- Compliance with Conditions of participation or other certification requirements
- Program participation and similar requirements
- Preapproval requirements
- Requirements that physicians and other health care professionals be licensed in the State in which they are providing services, so long as they have equivalent licensing in another State (this waiver is for purposes of Medicare, Medicaid, and CHIP reimbursement only – state law governs whether a non-Federal provider is authorized to provide services in the state without state licensure)
- Stark self-referral sanctions
- Performance deadlines and timetables may be adjusted (but not waived) (i.e. quality measure data submission)
- Sanctions and penalties arising from noncompliance with HIPAA privacy regulations relating to: a) obtaining a patient’s agreement to speak with family members or friends or honoring a patient’s request to opt out of the facility directory, b) distributing a notice of privacy practices, or c) the patient’s right to request privacy restrictions or confidential communications
- Limitations on payment for health care items and services furnished to Medicare Advantage enrollees by non-network providers
Waivers under section 1135 of the Social Security Act usually expire at the end of the emergency period or after 60 days, unless extended by the HHS Secretary for additional 60-day periods. Also, Medicare coverage or payment rules generally cannot be waived, even in a disaster or emergency.
Providers can request an 1135 waiver individually or in coordination with professional organizations in their area or at state and national levels. Submit 1135 waiver or other relief requests via the CMS 1135 Waiver web portal at CMS PHE Emergency Web Portal.
Hurricane Season Lessons Learned
The bottom line is that the incidence of disasters and emergencies are going up, resources and support are going down, and your preparedness and resiliency may be the key factor for success. Learning from your emergency plan implementations and outcomes helps build a stronger emergency plan and nurtures preparedness in your staff. Here are important 50,000-foot lessons learned for your consideration.
- Keep preparedness as a top organizational priority
- Add public health to all health care provision activity
- Collaborate across the community to build partnerships
- Incorporate technology into daily practice (i.e., electronic communication)
- Incorporate population factors into emergency planning
- Be nimble & forward thinking related to innovative staffing models
- Think about provision of quality of care in different ways – harness your creativity
- Listen to your staff – they are a ready source for innovative ideas
- Ingenuity and standardization are complements, not antagonists
- Implementation of creative ideas can be fast and effective
- Resourcefulness benefits from collaborations with diverse stakeholders
- Take care of your staff – they are your greatest resource
Stay nimble, strong, and compliant during this hurricane season and beyond.